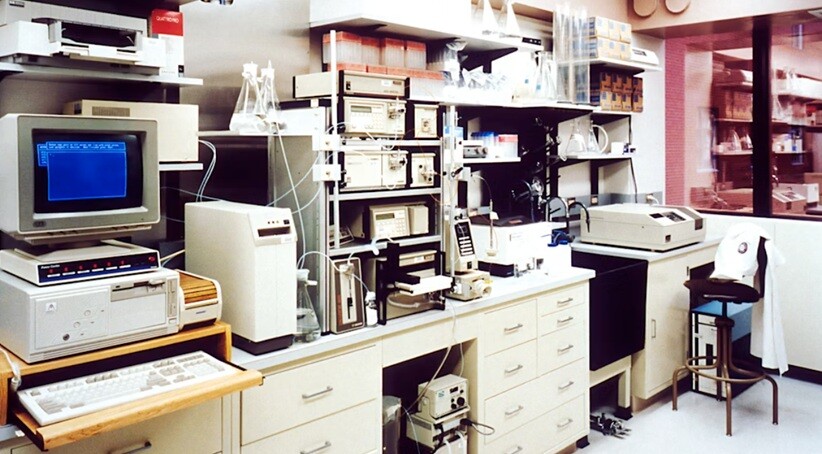
Translational research acts as the essential bridge connecting laboratory breakthroughs to clinical treatments that actually help patients. Yet despite massive investments in preclinical studies, there’s still a frustrating gap between promising lab results and successful clinical outcomes. This disconnect usually stems from shortcomings in how studies are designed, which models get chosen, and whether the methodologies truly capture the complexity of human disease. Closing this gap requires thoughtful planning and implementing best practices that bring laboratory work closer to clinical realities.
1. Implement Humanized and Patient-Derived Models
The animal models you choose fundamentally shape whether your preclinical research will translate to human applications. Traditional inbred mouse strains offer reproducibility and genetic consistency, but they often miss the genetic diversity and variability that define human populations. Humanized mice, engineered with human immune systems, tissues, or specific gene variants, provide vastly better platforms for investigating disease mechanisms and treatment responses that are truly human-specific. Patient-derived xenograft models take this further by transplanting tumor samples directly from patients into immunocompromised mice, preserving the intricate genetic landscape and microenvironmental characteristics of the original tumors.
2. Prioritize Clinically Relevant Endpoints and Biomarkers
Measuring outcomes that directly align with clinical assessments dramatically strengthens how well your preclinical work translates to the clinic. Too many preclinical studies focus on surrogate endpoints or mechanistic readouts that might be scientifically intriguing but don’t connect clearly to what matters for patients, things like survival, quality of life, or functional improvement. Establishing measurement protocols that mirror clinical trial endpoints creates direct comparability between your preclinical data and what clinicians will eventually see. Using validated biomarkers already established in clinical settings enables smoother transitions of findings across research phases and simplifies regulatory approval processes.
3. Apply Rigorous Experimental Design and Statistical Methods
Methodological rigor sits at the foundation of translational research that produces reliable, reproducible findings. Randomization procedures prevent selection bias and ensure treatment groups are truly comparable at baseline, the same gold-standard approach used in clinical trials. Blinding investigators to treatment assignments during data collection and analysis eliminates conscious or unconscious bias that might skew results toward expected outcomes. Sample size calculations based on statistical power analysis ensure your studies have enough sensitivity to detect clinically meaningful effects without wasting research resources. When conducting multi-phase drug development studies, researchers who partner with specialized preclinical research services can implement preregistration protocols where study designs and analysis plans are documented before any data collection begins, enhancing transparency and reducing selective reporting. Multi-site validation studies that replicate findings across different laboratories and research environments build confidence in how robust and generalizable your results really are. These methodological enhancements elevate preclinical research from exploratory investigations to definitive studies that meet the high evidentiary standards required for clinical translation.
4. Account for Biological Variables Including Sex and Age
The biological diversity within patient populations demands that preclinical studies incorporate relevant demographic and physiological variables to maximize translational accuracy. Historically, researchers have over-relied on young male animals, creating substantial knowledge gaps about sex-specific disease mechanisms and treatment responses that only become apparent during clinical trials. Including both male and female subjects in preclinical studies reveals sex-dependent differences in pharmacokinetics, immune responses, and disease susceptibility that critically inform clinical development strategies. Age-matched models that reflect the typical patient population for specific diseases provide much more accurate predictions of therapeutic efficacy and safety profiles.
5. Optimize Dosing Regimens and Treatment Schedules
Translational disconnect frequently emerges when there’s a mismatch between preclinical dosing strategies and what’s actually feasible in clinical settings. Preclinical studies often employ dosing regimens optimized for experimental convenience rather than clinical practicality, which leads to efficacy demonstrations that can’t be replicated in patients. Allometric scaling approaches that account for differences in metabolic rates between species enable more accurate translation of effective doses from animals to humans. Pharmacokinetic and pharmacodynamic modeling provides mechanistic understanding of dose-response relationships and helps identify optimal therapeutic windows.
6. Integrate Multi-Disciplinary Expertise and Collaborative Networks
Complex translational challenges require diverse expertise spanning basic biology, clinical medicine, biostatistics, and regulatory science, no single researcher can master it all. Establishing collaborative research teams that include clinician-scientists ensures that preclinical study designs address clinically relevant questions and incorporate practical considerations for eventual patient application. Engaging regulatory affairs specialists during preclinical stages helps researchers understand approval pathways and generate data packages that actually meet regulatory requirements. Biostatistician involvement from study inception through analysis guarantees appropriate statistical approaches and prevents common methodological pitfalls that can undermine data quality.
7. Establish Transparent Reporting and Data Sharing Practices
Scientific transparency and open data practices fundamentally strengthen the translational research enterprise by enabling critical evaluation, replication, and meta-analysis of preclinical findings. Comprehensive reporting of methodological details, including animal characteristics, experimental conditions, and complete statistical analyses, allows other researchers to assess study quality and attempt replication. Adherence to reporting guidelines such as ARRIVE ensures essential information gets consistently documented, which facilitates meaningful comparisons across different studies. Public registration of preclinical studies in accessible databases reduces publication bias by documenting both positive and negative results, something journals have historically discouraged.
Conclusion
Enhancing translational relevance in preclinical research represents both a scientific imperative and an ethical obligation to maximize the return on investment in biomedical research. The seven strategies outlined above provide actionable frameworks for improving how well preclinical studies predict clinical outcomes and increasing the probability of clinical success. Implementation requires genuine commitment from researchers, institutions, funding agencies, and publishers to prioritize methodological rigor, biological relevance, and transparent practices over convenience or convention. While no single approach guarantees translational success, systematically applying these principles significantly strengthens the foundation upon which clinical advances get built.
You may also like to read,
- Enhancing Clinical Decisions Through Innovative Healthcare Data Models
- In-House laboratory Services you can Expect at an Emergency Room
- The point of action and testing for different viruses